Central Sleep Apnea – South Portland
A Less Common Sleep Disorder

Most of the time, when you hear about sleep apnea, the discussion surrounds obstructive sleep apnea (OSA). OSA is a common sleep disorder that affects approximately 22 million Americans. However, many people don’t know that there is another type of sleep apnea that can also have dire effects: central sleep apnea (CSA). Continue reading to learn more about this condition and how it works.
What Is Central Sleep Apnea?

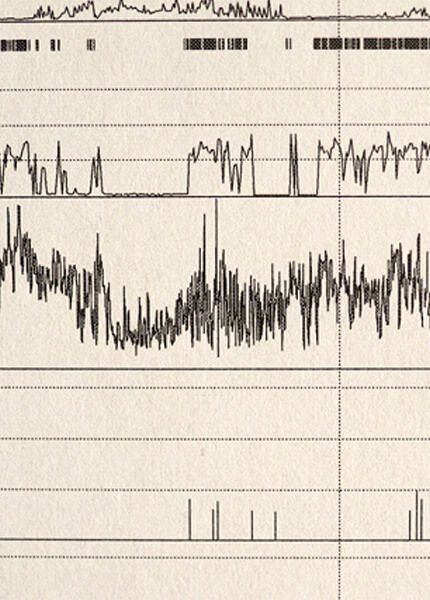
OSA and CSA both consist of repetitive cessions in breathing throughout the night, and they have similar symptoms. The difference is what causes these cessions. Obstructive sleep apnea is caused by the tissues in the upper airway relaxing and “obstructing” the free flow of air. On the other hand, central sleep apnea occurs when the brain isn’t sending the correct signals to the muscles that control breathing.
What Causes Central Sleep Apnea?

There are a variety of possible causes of CSA. Here are some of the most common:
- Cheyne-Stokes Breathing: This condition is apparent in about half of all CSA cases. It is defined as a cycle when a person’s breathing speeds up, slows down, stops, and then starts again.
- Medications: Narcotic medications, including oxycodone and morphine, can affect your breathing patterns.
- High Altitude: Central sleep apnea is more common at higher altitudes – usually above 8,000 feet.
- Medical Conditions: Medical conditions, like kidney failure, heart failure, and stroke can all increase your risk of CSA.
Possible Complications of Central Sleep Apnea

CSA is associated with numerous serious health conditions. Some of them include:
- Irregular Heartbeat
- High Blood Pressure
- Obesity
- Diabetes
- Heart Failure
- Heart Attack
- Stroke
If you have one of the conditions listed above, having CSA can worsen them, putting you at higher risk.
When Should You See a Doctor?
If you are concerned about your quality of sleep, or your significant other has noticed that your breathing stops at night, this warrants a visit to your doctor. You can discuss your symptoms and see if the next steps need to be taken, like undergoing a sleep test. Once you receive a diagnosis, you can work together to find a treatment plan that works best for you. For some, an adjustment of medication is enough to make a difference while others may require an oral appliance or combined therapy. By seeking help from a professional, you can work on getting the quality sleep you need to thrive!

